Anatomy of a Pandemic webinar series: Striking a balance between infection and isolation in long-term care
By Shefali Rai, November 29 2020—
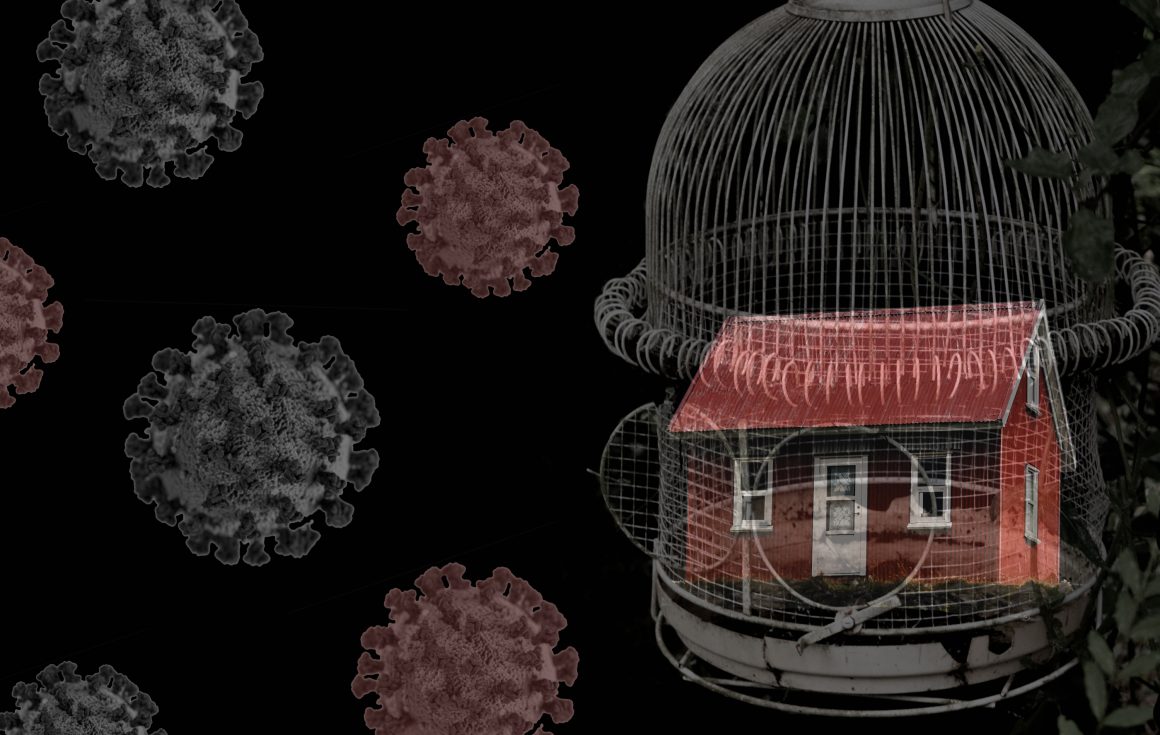
By now, we’ve all read countless articles related to COVID-19 and been advised to follow even more protocols to “flatten the curve.” As tired as we all are with this rhetoric, we are still grappling with surging COVID-19 cases — especially in Alberta. So where is the disconnect?
As it turns out, roughly 60 percent of our active cases are from people under the age of 40. On the flip side almost 90% of the mortality rates linked to COVID-19 are from our older populations — aged 70 or over. While our grandparents and aging loved ones take the brunt of this pandemic, the ever-increasing threat to mental wellbeing from lockdown procedures and restrictions in long-term care facilities are far more feared. The O’Brien Institute for Public Health and the Brenda Strafford Centre on Aging hosted a digital forum to incorporate multiple perspectives on these issues as our province enters its second wave.
Dr. David Hogan, Academic Lead of the Brenda Strafford Centre on Aging, began the forum by stating that, “there needs to be a balance between individual rights and communal good.”
How do we stop the spread of infection without restricting and inadvertently harming an entire population? Do we isolate our loved ones for their own protection? Is enforcing another lockdown a necessary evil? Keynote speakers Dr. Craig Jenne, Associate Professor and Infectious Disease Specialist at the University of Calgary, and Lisa Poole, Family Care Partner, addressed these concerns during the forum.
Within our senior populations, 81 percent of all COVID-19 deaths in Canada are attributed to residents of long-term care or supportive living facilities. This chilling statistic was echoed by every single panelist and speaker throughout the forum.
Jenne explained, “the problem is [that] the burden of disease is not born evenly. Younger people make up the majority of cases… [but] it is disproportionately affecting older Canadians. [So] how do we keep the virus out?”
A seemingly appealing answer is to lock down long-term care facilities, however Jenne exposes several problems with that approach.
Aside from the ethical and psychological implications, Jenne emphasized “it’s impossible to lock down a facility. If we look at hospitals — [where] staff are fully trained in infection control, have PPE and protocols — [they] should be able to limit the spread. Even with all of those controls in place, 13 acute care facilities had outbreaks in the province. Sealing off a facility is simply not a feasible approach…[even] from just a mechanistic point of view.”
Poole added that, “numbers matter but so does quality of life.” Each number in a statistic that we gloss over is someone’s father, great aunt, or grandmother.
Poole’s father, John, who has vascular dementia, lives in a long-term care facility much like thousands of Canadians. Throughout the country residents are experiencing confinement syndrome – a phenomenon similar to solitary confinement in prison. Poole’s father also felt this overwhelming devastation from being completely separated from his family during a recent outbreak. Poole reminds us of the human side of this pandemic, empowering us to acknowledge the essential role of family care partners to provide physical, emotional and social support.
In a follow-up interview with Poole, she recognizes that this may not be an issue on any of our radars – unless we have a family member in a long-term care facility.
She expressed that “we all have a role to play in trying to get the virus out of our lives. The younger generation [especially will] be impacted by the amount of money we’re spending on COVID. Washing your hands, being mindful of staying away from people and trying to reduce spread of the virus is an investment in your own future.”
Poole said “families can and want to be part of the solution. We want to be recognized as essential partners in care. If cases continue to rise, [we must] resist the urge to only look through the lens of infection control.”
Also weighing in on this topic was an esteemed panel of experts — Wayne Morishita, Executive Director for Alberta Continuing Care Association (ACCA), Dr. Vivian Ewa, Medical Director Facility Living for Alberta Health Services and Dr. Jim Silvius, Provincial Medical Directors Seniors for Alberta Health Services (AHS). They gathered together to remind us of the unity and tremendous effort arising from the current policies and measures being placed in Alberta. The take home message behind all their efforts – employ measures to keep our senior and long-term residents safe without isolating them.
“[We have] grieved over the loss of connection, not only the loss of life,” said Morishita. He understands it might be easy to get demoralized with our current situation but offers a different tale from the operators of the ACCA.
To combat this tragedy, Morishita explains how many operators have implemented creative solutions to keep families connected – heated trailers for cold weather visitations, social media adoption to keep loved ones engaged, organizing vintage car parades and placing exterior decorations on their facilities.
Both Ewa and Silvius highlight the risk-based approach from the current order — Chief Medical Officer of Health Order 29 — that introduces key measures like safe touch and supports long-term care residents without impeding on their freedoms.
Silvius also drew attention to the new Know Your Role and Know Your Risk documentation provided by AHS, stating that “[these documents] try to identify risk for unknown exposure and persuade [designated family and support persons] that they need to look at what they’re doing outside of their setting and modify their behaviors to reduce risk.”
“We all need to understand the risks. Let’s make sure family members are educated. [Implement] one-worker one-site policy, improve overall conditions for staff, bring in LPNs and RNs. Let’s all be prepared,” proclaimed Poole.
Public health officials might be the ones responsible for creating measures that can appropriately balance between achieving infection control and minimizing isolation, but we are all at the center of this issue and need to play our part if we want to see COVID-19 come to an end.
You can view the event recording here or browse the rest of the Anatomy of a Pandemic webinar series on the UCalgary website.
