Strides made at U of C to treat stroke survivors
By Erin Novakowski, March 23 2020—
with files from Nikayla Goddard
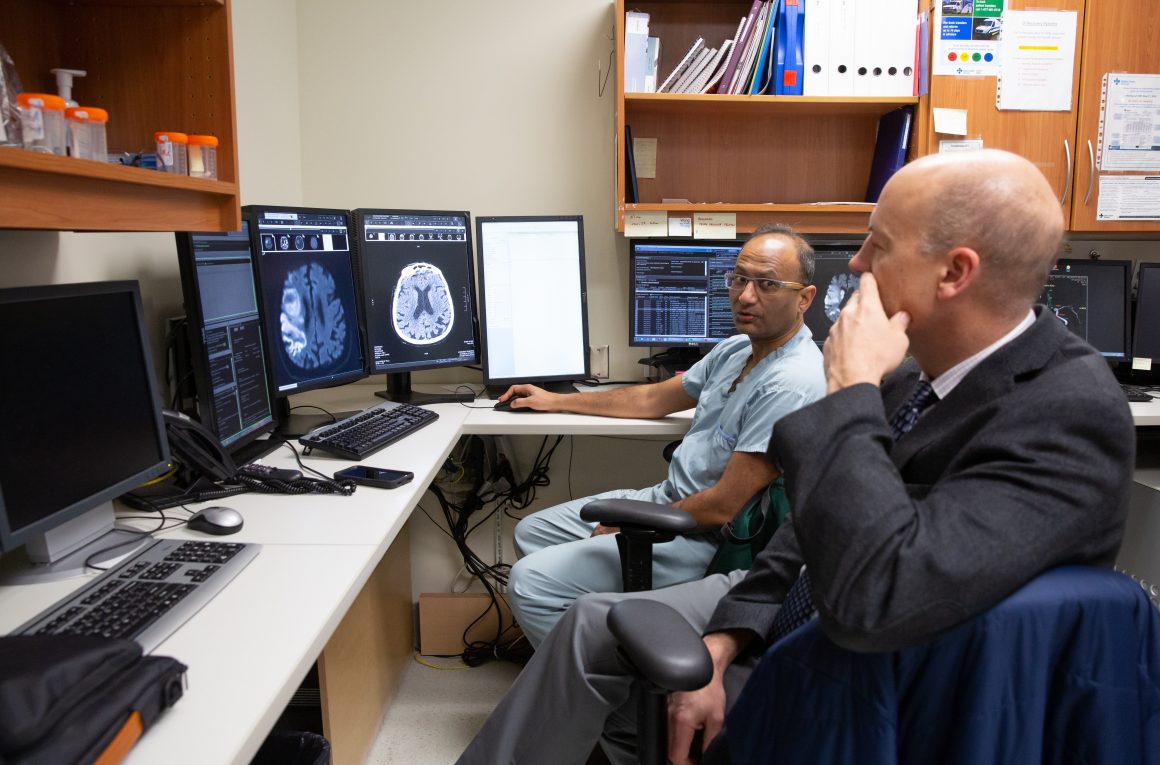
Thanks to the University of Calgary’s Cumming School of Medicine (CSM), big strides are being made in the treatment of stroke survivors and doctors’ ability to preserve patients’ brain cells. Michael Hill is a neurologist at Foothills Medical Centre and a professor of Clinical Neurosciences and Radiology in the CSM, and Mayank Goyal is a neuroradiologist at Foothills and a professor of Radiology. The two have been working collaboratively with a team that includes academics from Calgary to Toronto, and have recently found a way to massively improve the recovery of stroke patients using a peptide treatment.
According to the Heart and Stroke Foundation of Canada, strokes occur when blood stops flowing to any part of the brain. Ischemic strokes, which are the focus of a study conducted by Hill and Goyal, happen because of blood clots or blockages in the brain vessels. Hundreds of thousands of Canadians experience strokes each year, which can lead to disability, paralysis or death. Research in the field is rapidly developing, however, largely thanks to dedicated teams like those from the Cumming School of Medicine.
A trial named ESCAPE-NA1 conducted by the team had two sets of patients, with 60 per cent receiving the new peptide called nerinetide along with the standard “clot-buster medicines,” and 30 per cent receiving only nerinetide. The results were significant — researchers found that the group receiving nerinetide alone benefited from an increased recovery rate and a decreased mortality rate. According to Hill, this kind of result means the “difference between somebody being in a nursing home and walking out of a hospital.”
“The magnitude of the benefit is quite large,” he points out. For patients participating in the trial, it is no doubt that the advances made by ESCAPE-NA1 are life changing.
While the findings are monumental, they weren’t exactly what researchers initially anticipated. “We did not expect the dramatic, black and white component,” Hill states. The possible drug interaction was designed into the study, but the fact that results would so distinctly show the difference between receiving both drugs and receiving only nerinetide was unforeseen.
The results of this study tells researchers that “the process of proceeding with neuroprotectionism,”— this treatment that allows doctors to preserve brain cells after a stroke— “is possible.” Hill believes it’s essential to continue gathering data on the subject and pursue more trials to verify the effectiveness of this very promising treatment.
“That’s […] a totally new finding,” Hill emphasizes. “It opens up a whole new potential world of therapeutics in neurological conditions. That’s the exciting part of it.”
Researchers believe that this form of treatment, if proven to be effective in strokes, may also be applicable to other neurological conditions. The study was a “Calgary-led international consortium,” and a “significant advance in understanding brain diseases.” Hill is hopeful that in the next 2-3 years, a new treatment will be available based on the research of this team.
While Hill and Goyal are regarded as the lead of the project, Hill makes it very clear that the work would not have been possible without the collaboration of everyone involved in the Calgary Stroke Program.
“These are huge team efforts. All of us are working together at an incredible pace,” he said.
